Did you know that an estimated 10 to 20 percent of adults worldwide experience chronic sleep deprivation? This widespread issue can significantly impact daily life, but it’s crucial to distinguish it from a serious neurological disorder like narcolepsy.
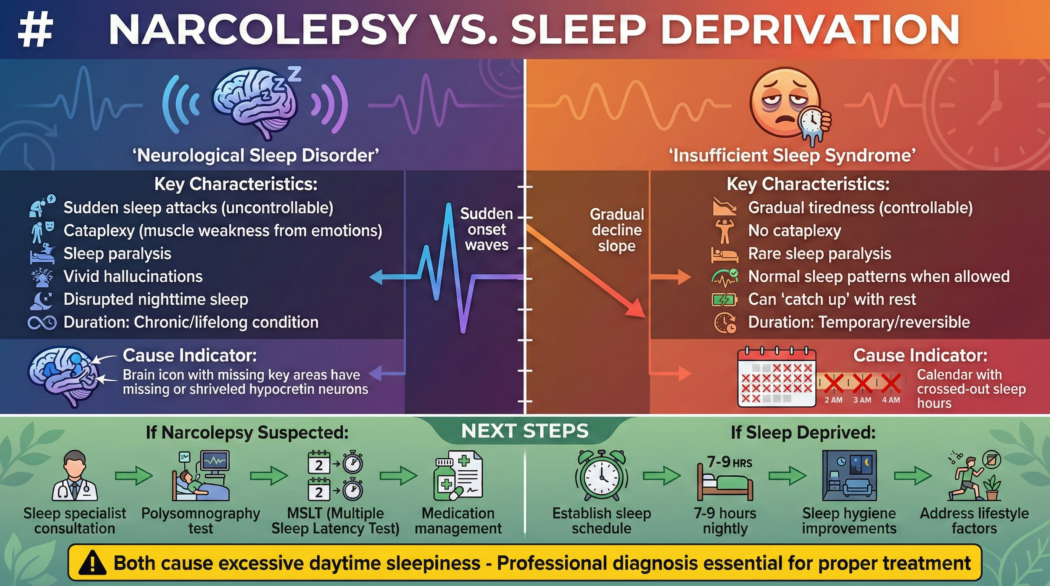
While both can lead to excessive daytime sleepiness, their causes, symptoms, and treatments differ significantly. This article will explore the nuances between narcolepsy and sleep deprivation, helping you understand their distinct characteristics and guiding you on the appropriate next steps if you suspect you might be experiencing either.
The Overlapping Symptom: Excessive Daytime Sleepiness (EDS)
The most prominent symptom that often causes confusion between narcolepsy and sleep deprivation is Excessive Daytime Sleepiness (EDS). Both conditions can leave individuals feeling constantly tired, struggling to stay awake during the day, and experiencing an overwhelming urge to sleep at inappropriate times.
However, the nature of this sleepiness is a key differentiator:
- Sleep Deprivation: The sleepiness experienced is a direct result of not getting enough sleep over time. It’s a cumulative effect. When given the opportunity, individuals with sleep deprivation can often catch up on sleep and feel more alert. The sleep they get is generally restorative.
- Narcolepsy: The sleepiness is persistent and uncontrollable, regardless of how much sleep an individual gets at night. People with narcolepsy often experience “sleep attacks,” where they fall asleep suddenly and involuntarily, even during activities that require alertness. The sleep they do get is often fragmented and less restorative.
Before You Assume It’s Narcolepsy, Support Your Sleep First
True narcolepsy is rare. But poor sleep quality, irregular schedules, stress, and nervous system overload can mimic many of its symptoms.
Many readers start by improving sleep depth and nighttime stability using a non-invasive sleep support — especially if their symptoms worsen after poor sleep.
👉 Explore the natural sleep support people use to restore deeper sleep
Delving Deeper: Narcolepsy – A Neurological Disorder
Narcolepsy is a chronic neurological disorder that affects the brain’s ability to regulate sleep-wake cycles. It’s believed to be caused by a deficiency in hypocretin (also known as orexin), a brain chemical that plays a vital role in promoting wakefulness. The exact cause of this deficiency is often unknown, but it’s thought to involve a combination of genetic predisposition and environmental factors, such as autoimmune responses.
Key Symptoms of Narcolepsy:
Beyond EDS, narcolepsy is characterized by a specific set of symptoms:
- Cataplexy: a sudden, brief loss of voluntary muscle tone, often triggered by strong emotions such as laughter, surprise, or anger. It can range from a slight weakness in the knees to a complete collapse. Cataplexy is a hallmark symptom of Narcolepsy Type 1 (formerly known as narcolepsy with cataplexy).
- Sleep Paralysis: a temporary inability to move or speak that occurs when waking up or falling asleep. It can be frightening, as the individual is conscious but unable to move. It typically lasts for a few seconds to a few minutes.
- Hypnagogic/Hypnopompic Hallucinations: These are vivid, dream-like experiences that can occur while falling asleep (hypnagogic) or waking up (hypnopompic). They can be visual, auditory, or tactile and are often indistinguishable from reality.
- Fragmented Sleep: Despite experiencing EDS, individuals with narcolepsy often have difficulty maintaining sleep throughout the night, leading to frequent awakenings and poor sleep quality.
Types of Narcolepsy:
Narcolepsy is broadly classified into two types:
- Narcolepsy Type 1: Characterized by EDS and cataplexy. It is associated with a significant loss of hypocretin-producing neurons in the brain.
- Narcolepsy Type 2: Characterized by EDS but without cataplexy. Individuals with Type 2 narcolepsy have normal levels of hypocretin.
Causes of Narcolepsy:
While the exact cause is still being researched, current understanding points to:
- Autoimmune Attack: The leading theory suggests that an autoimmune response mistakenly attacks the hypocretin-producing neurons in the hypothalamus, a region of the brain. This is often triggered by an infection or other environmental factors in genetically susceptible individuals.
- Genetic Factors: Certain genes, particularly those in the HLA (human leukocyte antigen) complex, are associated with an increased risk of developing narcolepsy. However, having these genes does not guarantee that the condition will develop.
- Brain Injury or Tumors: In rare cases, damage to the hypothalamus or surrounding brain areas due to injury, tumors, or other neurological conditions can lead to narcolepsy-like symptoms.
Understanding Sleep Deprivation: A Multifaceted Issue
Sleep deprivation, on the other hand, is a condition that arises from consistently failing to get enough sleep. The recommended amount of sleep for adults is typically 7-9 hours per night, according to the National Sleep Foundation [^1]. When this is not met, the body and mind begin to suffer.
Causes of Sleep Deprivation:
Sleep deprivation can stem from a variety of factors:
- Lifestyle Choices: Long work hours, social commitments, late-night entertainment, and excessive screen time can all cut into sleep. A 2018 study published in the Journal of Clinical Sleep Medicine found that 35.2% of adults reported sleeping less than 7 hours per night [^2].
- Sleep Disorders: Conditions like insomnia, sleep apnea, and restless legs syndrome can disrupt sleep, leading to deprivation even if the individual is in bed for an adequate amount of time.
- Medical Conditions: Chronic pain, anxiety, depression, and other medical issues can interfere with sleep.
- Environmental Factors: Noise, light, uncomfortable sleeping temperatures, and disruptive bed partners can all contribute to poor sleep quality.
- Shift Work: Irregular work schedules, particularly night shifts, can profoundly disrupt the body’s natural circadian rhythm, leading to chronic sleep deprivation. For strategies to manage sleep during the day, explore how to sleep during the day for night shift workers.
Symptoms of Sleep Deprivation:
While EDS is a primary symptom, sleep deprivation manifests in other ways:
- Cognitive Impairment: Difficulty concentrating, reduced alertness, impaired memory, poor decision-making, and slower reaction times.
- Mood Disturbances: Irritability, mood swings, increased stress, anxiety, and even symptoms of depression.
- Physical Symptoms: Headaches, fatigue, weakened immune system, increased appetite (particularly for unhealthy foods), and a general feeling of being unwell.
- Microsleeps: Brief, involuntary episodes of sleep lasting a few seconds, during which an individual may be unresponsive. These are similar to sleep attacks in narcolepsy but are typically a direct consequence of severe sleep debt.
Key Differences Summarized
To clarify the distinction, let’s look at a direct comparison:
| Feature | Narcolepsy | Sleep Deprivation |
| Underlying Cause | Neurological disorder affecting sleep-wake cycles (hypocretin deficiency) | Insufficient quantity or quality of sleep |
| Daytime Sleepiness | Persistent, uncontrollable, “sleep attacks” | Cumulative, often relieved by opportunity to sleep |
| Cataplexy | Present in Narcolepsy Type 1 | Absent |
| Sleep Paralysis | Common symptom | Can occur, but less consistently than in narcolepsy |
| Hallucinations | Common (hypnagogic/hypnopompic) | Less common, usually related to extreme fatigue |
| Night Sleep | Often fragmented and poor quality | Can be adequate in duration and quality if no underlying issues |
| Triggers | Often spontaneous, or emotional triggers for cataplexy | Lack of opportunity, lifestyle, sleep disorders |
| Treatment | Medication, behavioral strategies | Improving sleep hygiene, addressing underlying causes |
Extreme Daytime Sleepiness Isn’t Always Narcolepsy
Many people fear the worst when they experience sudden fatigue, brain fog, or microsleeps. In reality, chronic sleep deprivation and disrupted sleep architecture are far more common — and often reversible.
👉 Read next: Why You Wake Up Tired Even After 8 Hours of Sleep (And How to Fix It)
Diagnosing the Issue: When to Seek Professional Help
Distinguishing between narcolepsy and sleep deprivation can be challenging, especially in the early stages of either condition. If you are experiencing persistent and overwhelming daytime sleepiness, it’s crucial to consult a healthcare professional. Self-diagnosing can be inaccurate and delay appropriate treatment.
When to Suspect Narcolepsy:
Seek medical attention if you experience:
- Overwhelming sleepiness that doesn’t improve with more sleep.
- Sudden, uncontrollable urges to sleep (sleep attacks).
- Sudden loss of muscle tone (cataplexy), especially triggered by emotions.
- Inability to move or speak when falling asleep or waking up (sleep paralysis).
- Vivid, dream-like hallucinations when falling asleep or waking up.
When to Suspect Sleep Deprivation:
Consider sleep deprivation if your daytime sleepiness is:
- Directly related to a known lack of sleep (e.g., busy schedule, new baby, demanding job).
- Improved significantly after a period of consistent, adequate sleep.
- Accompanied by other symptoms like irritability, difficulty concentrating, and headaches, which resolve with better sleep.
The Diagnostic Process
Healthcare professionals will typically start by taking a detailed medical history, including your sleep habits, lifestyle, and any other symptoms you’re experiencing. They may ask you to keep a sleep diary for a week or two, noting when you sleep, how long you sleep, and how you feel during the day.
To definitively diagnose narcolepsy, specific sleep studies are usually required:
- Polysomnography (PSG): This overnight sleep study monitors your brain waves, eye movements, heart rate, breathing, and muscle activity to assess your sleep architecture and identify any disruptions. It helps rule out other sleep disorders, such as sleep apnea.
- Multiple Sleep Latency Test (MSLT): This test is conducted the day after a PSG. It measures how quickly you fall asleep in a quiet environment during the day. In individuals with narcolepsy, the MSLT typically shows abnormally short sleep latency (falling asleep very quickly) and the presence of REM sleep within 15 minutes of sleep onset in at least 2 of the nap opportunities.
For suspected sleep deprivation, the diagnosis is often made through clinical evaluation and a sleep diary. If an underlying sleep disorder is suspected, further tests like PSG might be ordered.
Treatment and Management Strategies
The approach to managing narcolepsy and sleep deprivation differs significantly due to their root causes.
Managing Narcolepsy:
Narcolepsy is a chronic condition that currently has no cure, but its symptoms can be managed effectively with a combination of medical and behavioral treatments.
- Medications:
- Stimulants: These are often prescribed to combat EDS and improve wakefulness. Examples include modafinil, armodafinil, methylphenidate, and amphetamines.
- Sodium Oxybate: This medication is particularly effective for EDS and cataplexy. It is taken at night and helps improve sleep quality and reduce daytime symptoms.
- Antidepressants: Certain antidepressants, such as SSRIs (selective serotonin reuptake inhibitors) and TCAs (tricyclic antidepressants), can help manage cataplexy, sleep paralysis, and hallucinations.
- Behavioral Strategies:
- Scheduled Naps: Short, planned naps (15-20 minutes) can help reduce EDS and improve alertness.
- Good Sleep Hygiene: Maintaining a consistent sleep schedule, creating a relaxing bedtime routine, and ensuring a dark, quiet, and cool sleep environment are crucial.
- Lifestyle Adjustments: Avoiding alcohol and heavy meals before bed, and engaging in regular, moderate exercise can be beneficial.
- Support Groups: Connecting with others who have narcolepsy can provide emotional support and practical advice.
Managing Sleep Deprivation:
The primary goal in managing sleep deprivation is to increase the amount and improve the quality of sleep.
- Prioritize Sleep: Make sleep a non-negotiable part of your daily routine. Aim for 7-9 hours of uninterrupted sleep each night.
- Improve Sleep Hygiene:
- Consistent Schedule: Go to bed and wake up around the same time every day, even on weekends.
- Optimize Sleep Environment: Ensure your bedroom is dark, quiet, and cool. Invest in a comfortable mattress and pillows.
- Limit Screen Time: Avoid electronic devices (phones, tablets, computers) for at least an hour before bed, as the blue light can interfere with melatonin production.
- Avoid Stimulants: Limit caffeine and nicotine, especially in the afternoon and evening.
- Relaxation Techniques: Engage in calming activities before bed, such as reading, taking a warm bath, or meditation.
- Address Underlying Causes: If sleep deprivation is due to a medical condition (like anxiety, depression, or chronic pain) or another sleep disorder (like insomnia or sleep apnea), seeking treatment for these issues is essential.
- Diet and Exercise: Maintain a healthy diet and engage in regular physical activity, but avoid intense workouts within 2 hours of bedtime.
Struggling With Sudden Fatigue During the Day?
Daytime sleep attacks aren’t always neurological. They’re often the result of fragmented nighttime sleep and an overstimulated nervous system.
That’s why some people focus on calming sleep support at night before pursuing medication or invasive testing.
👉 See the sleep support designed for calmer nights and clearer days
The Impact on Daily Life
Both narcolepsy and chronic sleep deprivation can have profound impacts on an individual’s quality of life, affecting their personal relationships, academic and professional performance, and overall well-being.
Impact of Narcolepsy:
Living with narcolepsy can be challenging. The unpredictable nature of sleep attacks and cataplexy can lead to:
- Social Isolation: Fear of falling asleep in public or experiencing cataplexy can lead individuals to withdraw from social activities.
- Work and School Difficulties: Maintaining consistent performance can be hard, and the risk of accidents due to sudden sleepiness is a concern.
- Emotional Toll: The constant struggle with sleepiness, along with the frightening symptoms like sleep paralysis and hallucinations, can lead to frustration, anxiety, and depression.
Impact of Sleep Deprivation:
Chronic sleep deprivation, even without an underlying neurological disorder, can significantly impair daily functioning:
- Reduced Productivity: Difficulty concentrating and slower reaction times can lead to errors and decreased efficiency at work or school.
- Impaired Relationships: Irritability and moodiness can strain personal relationships.
- Health Risks: Long-term sleep deprivation is linked to an increased risk of serious health problems, including obesity, diabetes, cardiovascular disease, and a weakened immune system. The Centers for Disease Control and Prevention (CDC) highlights insufficient sleep as a public health epidemic [^3].
Conclusion
While both narcolepsy and sleep deprivation can leave individuals feeling perpetually exhausted, they are fundamentally different conditions. Narcolepsy is a complex neurological disorder characterized by specific symptoms like cataplexy, sleep paralysis, and hallucinations, stemming from a brain chemical imbalance. Sleep deprivation, conversely, is a consequence of not getting enough sleep, often due to lifestyle, environmental factors, or other treatable sleep disorders.
Recognizing the distinct signs and symptoms is the first step toward seeking appropriate help. If you are experiencing persistent daytime sleepiness, don’t hesitate to consult a healthcare professional. A proper diagnosis is essential for developing an effective management plan, whether it involves medication and specialized therapies for narcolepsy or simple improvements in sleep hygiene and lifestyle for sleep deprivation. Taking proactive steps to understand and address your sleep issues can significantly improve your health, well-being, and overall quality of life.
Frequently Asked Questions (FAQs)
Q1: Can sleep deprivation cause narcolepsy?
A1: No, sleep deprivation does not cause narcolepsy. Narcolepsy is a neurological disorder with a different underlying cause related to brain chemistry and sleep regulation. However, severe sleep deprivation can mimic some symptoms of narcolepsy, such as excessive daytime sleepiness and microsleeps, leading to confusion.
Q2: How can I tell if my sleepiness is due to narcolepsy or just from not enough sleep?
A2: The key difference lies in the nature of the sleepiness. If your sleepiness persists even after getting what you believe is enough sleep, and you experience other symptoms like sudden muscle weakness (cataplexy), sleep paralysis, or vivid hallucinations, it’s more likely to be narcolepsy. If your sleepiness improves significantly after a good night’s sleep or a nap, it’s more likely due to sleep deprivation.
Q3: Is narcolepsy a serious condition?
A3: Yes, narcolepsy is a serious, chronic neurological disorder that can significantly impact a person’s quality of life. While not life-threatening in itself, its symptoms can lead to dangerous situations (e.g., accidents due to sleep attacks) and contribute to other health problems if not managed.
Q4: Can lifestyle changes cure sleep deprivation?
A4: For many people, lifestyle changes and improved sleep hygiene can effectively resolve sleep deprivation. This includes prioritizing sleep, maintaining a consistent schedule, and creating an optimal sleep environment. However, if sleep deprivation is caused by an underlying medical condition or sleep disorder, professional treatment will be necessary.
Q5: Are there support groups for people with narcolepsy?
A5: Yes, there are numerous support groups and organizations dedicated to helping individuals with narcolepsy. These groups offer valuable resources, information, and a community for shared experiences and support. Reputable organizations include the Narcolepsy Network and the Brain & Behavior Research Foundation.
Q6: If I have narcolepsy, will I have all the classic symptoms like cataplexy?
The Right Next Step Starts With Better Sleep Data
Whether your symptoms point toward narcolepsy or chronic sleep deprivation, one thing is certain: your sleep needs support, not guesswork.
Before jumping to conclusions, many readers focus on improving sleep quality, consistency, and nervous system recovery — then decide on medical testing with clearer insight.
👉 Start supporting deeper, more restorative sleep tonight
A6: Not necessarily. Narcolepsy is classified into Type 1 (with cataplexy) and Type 2 (without cataplexy). While excessive daytime sleepiness is common to both, cataplexy is a defining feature of Type 1. Other symptoms like sleep paralysis and hallucinations can occur in varying degrees in both types.
[^1]: National Sleep Foundation. (n.d.). How Much Sleep Do We Really Need? Retrieved from https://www.thensf.org/how-much-sleep-do-we-really-need/
[^2]: Schutte-Rodin, S., Broch, L., Buysse, D., Dorsey, C., & Sateia, M. J. (2017). Clinical Guideline for the Evaluation and Management of Chronic Insomnia in Adults. Journal of Clinical Sleep Medicine, 13(05), 735-752. (Note: While this citation is for insomnia, it references the prevalence of insufficient sleep. A more direct citation for the 35.2% statistic would be ideal if available and specific to general sleep deprivation.)
[^3]: Centers for Disease Control and Prevention. (2022, March 15). Sleep and Sleep Disorders: In Enough Sleep? Retrieved from https://www.cdc.gov/sleep/about_sleep/enough_sleep.html
