For many people, sleep problems don’t begin in the bedroom — they begin in the stress response system.
You may feel physically exhausted but mentally alert. You go to bed on time, avoid screens, and still find yourself awake. Or you fall asleep quickly, then wake at 2 or 3 a.m. with your mind racing and your heart pounding.
These patterns are classic signs of stress-driven circadian disruption, where the hormone cortisol interferes with the body’s natural sleep–wake rhythm.
Understanding how cortisol, stress, and sleep interact helps explain why insomnia often persists despite good sleep hygiene, and why solutions that ignore stress biology often fail.
What Is Cortisol and Why Does It Matter for Sleep
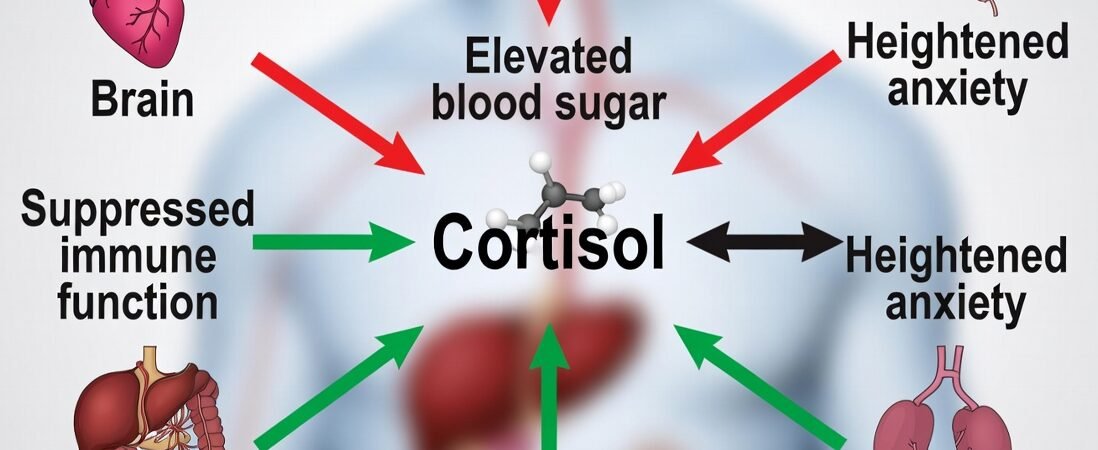
Cortisol is a hormone produced by the adrenal glands that regulates alertness, energy availability, and the body’s response to stress. Cortisol does not act alone. Sleep regulation depends on interconnected systems involving stress hormones, neurotransmitters, and the microbiome. This interaction is often described through the gut–brain axis and sleep regulation, which plays a central role in circadian stability and sleep quality.
In healthy individuals, cortisol follows a circadian rhythm—highest in the morning to promote wakefulness and lowest at night to allow sleep.
- Regulating energy and blood sugar
- Supporting immune function
- Mobilizing the body during stress
- Coordinating circadian rhythm
Under healthy conditions, cortisol follows a daily rhythm:
- Highest in the morning, helping you wake up alert
- Gradually declining throughout the day.
- Lowest at night, allowing melatonin and sleep pressure to rise
This rhythm opposes melatonin. When cortisol stays elevated late into the evening, sleep becomes difficult even when melatonin is present.
The HPA Axis: How Stress Hormones Control Sleep–Wake Cycles
Cortisol production is regulated by the hypothalamic–pituitary–adrenal (HPA) axis, a central stress response system that connects the brain and adrenal glands.
When the brain perceives stress, whether physical, emotional, or psychological, the HPA axis activates and releases cortisol to prepare the body for action.
Short-term activation is adaptive. Chronic activation is not.
Persistent stress keeps the HPA axis “on,” flattening normal cortisol rhythms and interfering with circadian signaling.
Why Cortisol Should Be Low at Night — but Often Isn’t
Under normal conditions, nighttime cortisol should fall to its lowest point, allowing the body to enter a state of repair. Chronic stress prevents this by:
- Delaying cortisol decline
- Increasing nighttime cortisol release
- Blunting the morning cortisol surge
- Flattening overall circadian amplitude
This leads to a state often described as “tired but wired.”
Even when the body is physically exhausted, elevated cortisol keeps the nervous system alert.
Nighttime Cortisol and “Wired but Tired” Insomnia
Elevated nighttime cortisol is strongly associated with:
- Difficulty falling asleep
- Frequent nighttime awakenings
- Early morning waking
- Reduced deep (slow-wave) sleep
- Increased sympathetic nervous system activity
This type of insomnia differs from sleep deprivation. It is not caused by lack of sleep opportunity — it is caused by biological hyperarousal.
Sedative sleep aids may induce unconsciousness, but they do not resolve the underlying stress signaling driving the problem.
How Chronic Stress Disrupts Circadian Rhythm and Melatonin
Cortisol and melatonin operate in a delicate balance.
When cortisol remains elevated:
- Melatonin secretion may be delayed.
- Melatonin signaling may become less effective.
- Sleep timing shifts later.
- Sleep architecture becomes fragmented.
This helps explain why many people find that melatonin initially works, then stops working over time — especially under ongoing stress.
Chronic stress does not just interfere with sleep onset; it reshapes circadian rhythm itself.
Read here → Why Melatonin Stops Working: Tolerance, Timing, and Gut Health
Stress, Gut Health, and the Cortisol–Microbiome Feedback Loop
Stress does not act solely on the brain. It directly affects the gut. As explored in greater depth in a previous post on microbiome-driven sleep regulation, stress-induced gut dysbiosis can amplify cortisol dysregulation and worsen sleep fragmentation.
Chronic cortisol elevation:
- Increases intestinal permeability
- Alters gut microbiota composition
- Increases inflammatory signaling
- Disrupts microbial circadian rhythms
In turn, gut dysbiosis feeds back into the stress response by:
- Altering neurotransmitter production (including serotonin)
- Increasing systemic inflammation
- Activating immune pathways that affect sleep regulation
This creates a self-reinforcing loop:
Stress disrupts the gut → gut disruption amplifies stress → sleep deteriorates further.
This is why addressing sleep without considering gut health often produces incomplete results.
Read here → pillar post on gut–brain–sleep regulation
Why Traditional Sleep Aids Don’t Fix Stress-Driven Insomnia
Sleep aids primarily target symptoms, not causes.
When cortisol is elevated:
- Sedatives may force sleep without restoring rhythm.
- Melatonin may be mistimed or overridden.
- Increasing doses often worsen grogginess.
- Sleep quality remains poor despite longer sleep duration.
Stress-driven insomnia is not a deficiency of sleep hormones — it is a misalignment of biological systems.
Restoring Sleep by Calming the Nervous System
Sustainable sleep improvement under chronic stress typically requires:
- Reducing sympathetic nervous system activation
- Supporting parasympathetic tone
- Stabilizing circadian rhythm
- Supporting gut health and inflammation balance
Rather than forcing sleep, these approaches focus on creating conditions that allow sleep to occur naturally.
For individuals whose insomnia is driven by stress, anxiety, or long-term circadian disruption, non-sedative approaches that emphasize calm and recovery may be more effective than traditional sleep aids.
When sleep problems are driven by chronic stress and elevated nighttime cortisol, forcing sleep often backfires. Approaches that focus on calming the nervous system and supporting circadian rhythm tend to be more sustainable.
Yu Sleep is designed for this exact scenario — supporting relaxation, parasympathetic activation, and deep sleep without relying on melatonin or sedatives.
👉 Read the evidence-based Yu Sleep review
Frequently Asked Questions
Can stress really cause long-term insomnia?
Yes. Chronic stress alters cortisol rhythms, nervous system balance, and circadian timing, all of which contribute to persistent sleep problems.
Why do I wake up in the middle of the night when stressed?
Elevated nighttime cortisol can trigger early awakenings and prevent return to sleep.
Is cortisol always bad for sleep?
No. Cortisol is essential for waking and daytime alertness. Problems arise when its rhythm is disrupted.
Does stress affect gut health and sleep at the same time?
Yes. Stress alters gut bacteria, inflammation, and neurotransmitter signaling, all of which influence sleep quality.
Can sleep improve without medication if stress is addressed?
For many people, yes. Supporting nervous system regulation and circadian rhythm often leads to meaningful improvements in sleep.
If you’re exhausted but feel wired at night, stress hormones—not sleep effort—may be the missing piece. We analyzed Yu Sleep through the lens of cortisol regulation, circadian rhythm, and real-world recovery data.
👉 Explore how Yu Sleep supports stress-driven sleep disruption
Final Thoughts: Sleep Problems Are Often Stress Problems
When sleep feels elusive despite doing “everything right,” the issue is often not effort — it is biology.
Chronic stress hijacks the circadian rhythm by dysregulating cortisol, activating the nervous system, and disrupting gut–brain feedback loops. Until these systems are addressed, sleep aids alone rarely provide lasting relief.
Understanding the role of cortisol reframes insomnia not as a failure to sleep, but as a signal that the body is stuck in survival mode.
Chronic stress doesn’t just make sleep harder — it changes how your body signals rest.
When cortisol stays elevated at night, sleep becomes lighter, shorter, and less restorative — no matter how tired you feel. The good news is that this pattern is reversible when you address the right systems, not just symptoms.
👉 Continue your sleep journey here to learn how nervous system regulation, circadian rhythm alignment, and targeted habits work together to restore deep, consistent sleep naturally.