Introduction
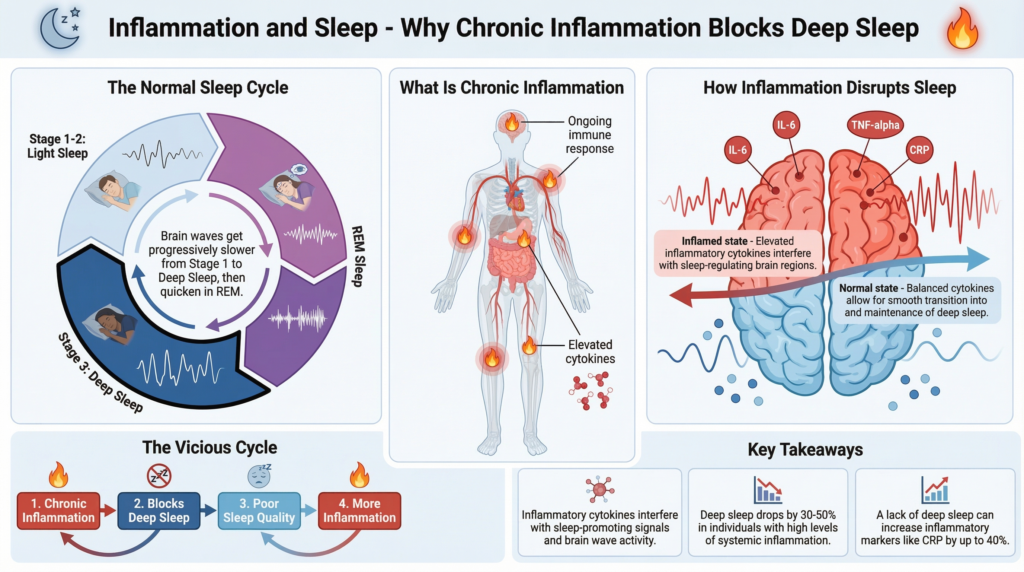
Sleep is often seen as a neurological or hormonal process, but chronic inflammation is another strong and often overlooked cause of poor sleep. More research shows that inflammation can disrupt deep sleep, throw off the circadian rhythm, and make it harder for the brain to enter restorative sleep phases.
Many people with insomnia, frequent night waking’s, or unrefreshing sleep think the problem is just melatonin, stress, or sleep habits. In fact, low-level chronic inflammation, often caused by gut health, stress, diet, or immune issues, may be quietly disrupting deep sleep.
To address sleep problems effectively, it’s important to understand how inflammation affects sleep, especially if usual strategies have not helped.
What Is Chronic Inflammation?
Inflammation is how the immune system responds to injury, infection, or stress. Acute inflammation is helpful and brief. Chronic inflammation happens when this response stays active at low levels for months or even years.
Common Drivers of Chronic Inflammation
- Gut microbiome imbalance (dysbiosis)
- Chronic psychological stress
- Poor sleep itself (a bidirectional loop)
- High-glycemic or ultra-processed diets
- Metabolic dysfunction
- Persistent immune activation
Research from the National Institutes of Health (NIH) shows that chronic inflammation is a key factor in many modern diseases, such as heart disease, metabolic problems, neurodegeneration, and more recently, sleep disorders.
How Sleep and Inflammation Are Biologically Connected
Sleep and the immune system are closely connected. During healthy sleep, especially deep sleep, the body lowers inflammation, which helps with tissue repair and resets the immune system.
When inflammation is high, the brain’s sleep centers, especially the hypothalamus, get mixed signals that interrupt normal sleep patterns.
Key Inflammatory Molecules That Affect Sleep
- Interleukin-6 (IL-6)
- Tumor Necrosis Factor-α (TNF-α)
- C-reactive protein (CRP)
NIH-funded studies show that elevated levels of IL-6 and TNF-α are associated with:
- Reduced deep sleep (N3)
- Increased nighttime awakenings
- Altered REM timing
- Daytime fatigue despite adequate sleep duration
Inflammation’s Impact on Deep Sleep (Slow-Wave Sleep)
Deep sleep is the most restorative phase of sleep. It is essential for:
- Immune regulation
- Hormonal balance
- Physical recovery
- Glymphatic (brain detoxification) activity
Chronic inflammation can disrupt deep sleep in several ways:
1. Disruption of Sleep Architecture
Inflammatory cytokines break up sleep cycles, so people spend less time in deep sleep even if they sleep for a normal amount of time.
2. Increased Sleep Pressure Without Restoration
Inflammation can make people feel sleepy but lowers sleep quality, so they wake up tired and not refreshed.
3. Impaired Nighttime Parasympathetic Activity
Inflammation pushes the nervous system into a more alert state, which keeps the brain from reaching deep sleep.
The Gut–Inflammation–Sleep Axis
The gut is a major source of chronic inflammation. The bacteria in the gut help control immune signals, inflammation, and even the production of brain chemicals.
When the gut barrier is weakened, sometimes called ‘leaky gut,’ inflammatory molecules like LPS can get into the bloodstream and trigger the immune system.
This process affects sleep directly through the gut-brain connection, which we cover in detail in our main guide on gut health and sleep.
How Gut-Driven Inflammation Affects Sleep
- Activates immune signaling pathways that suppress deep sleep
- Alters serotonin availability (a precursor to melatonin)
- Increases nighttime cortisol output
- Disrupts circadian rhythm signaling
Inflammation, Cortisol, and Circadian Rhythm
Chronic inflammation and stress are closely connected. Inflammation activates the HPA axis, which raises cortisol levels, especially at night.
Elevated nighttime cortisol:
- Delays sleep onset
- Reduces deep sleep duration
- Promotes early morning awakenings
This creates a cycle in which poor sleep leads to increased inflammation, which in turn further disrupts the body’s natural sleep rhythm. If you’re interested in this topic, also explore our article on cortisol, stress, and sleep disruption.
Why Inflammation Makes Sleep Fragmented
Sleep fragmentation, or frequent brief awakenings during the night, is a common but often overlooked result of chronic inflammation.
Mechanisms Behind Fragmented Sleep
- Cytokine signaling interferes with thalamic gating (sensory filtering during sleep)
- Increased sympathetic nervous system activity
- Reduced melatonin sensitivity at the cellular level
As a result, people may sleep for 7 to 8 hours but still wake up feeling tired, mentally foggy, and physically drained.
Diet, Inflammation, and Sleep Quality
What you eat has a big impact on inflammation. Diets high in refined carbs, omega-6 fats, and processed foods can raise inflammation and disrupt sleep.
On the other hand, eating an anti-inflammatory diet can help you sleep more deeply and consistently.
Sleep-Supporting Anti-Inflammatory Nutrients
- Soluble fiber (supports gut bacteria)
- Polyphenols (berries, olive oil)
- Omega-3 fatty acids
- Magnesium-rich foods
Prebiotic fibers are especially helpful because they feed good gut bacteria and lower inflammation. We explain this more in our article on prebiotics and sleep.
Why Anti-Inflammatory Sleep Support Matters More Than Sedation
Many people try to fix sleep problems caused by inflammation with sedatives or high doses of melatonin. These methods may make you sleepy, but they do not solve the root cause of inflammation.
Research shows that sleep from sedatives does not provide the same immune benefits as natural deep sleep.
Effective sleep support in the context of inflammation focuses on:
- Calming immune signaling
- Supporting parasympathetic nervous system activity
- Restoring circadian alignment
That’s why methods that help regulate the nervous system and prepare the body for sleep are usually more effective in the long run.
When to Consider Targeted Sleep Support
If inflammation is contributing to your sleep issues, common signs include:
- Feeling wired but exhausted
- Frequent night waking’s
- Poor recovery despite long sleep duration
- Sensitivity to stress or overtraining
- Limited benefit from melatonin
In these situations, sleep strategies that relax the nervous system, instead of forcing sleep, may work better. When sleep problems persist despite good sleep habits, the issue is often not sleep itself—but how the nervous system and immune signaling behave at night. In these cases, support that focuses on calming stress pathways and restoring circadian balance tends to be more effective than sedatives or high-dose melatonin.
We evaluated Yu Sleep through the lens of inflammation, stress physiology, and real-world recovery data to understand where it fits in this context.
👉 Read the evidence-based Yu Sleep review
Frequently Asked Questions (FAQ)
Does inflammation cause insomnia?
Yes. Chronic inflammation is strongly associated with insomnia, interrupted sleep, and reduced deep sleep, driven by immune signaling that disrupts sleep architecture.
Can reducing inflammation improve sleep?
Studies suggest that lowering inflammatory markers through diet, stress reduction, and gut health support can notably improve sleep quality and depth.
Is poor sleep inflammatory?
Absolutely. Sleep deprivation increases inflammatory cytokines, creating a vicious cycle between poor sleep and immune activation.
Does melatonin reduce inflammation?
Melatonin has mild anti-inflammatory properties, but inflammation can also impair melatonin signaling, limiting its effectiveness in chronic cases.
What helps improve deep sleep when inflammation and stress are high?
Improving deep sleep in the context of chronic inflammation often requires calming the nervous system and supporting circadian rhythm rather than forcing sleep with sedatives. Strategies that reduce nighttime stress signaling and promote parasympathetic activity tend to be more effective long-term.
Read the evidence-based Yu Sleep review
How does gut health affect inflammation and sleep?
The gut microbiome regulates immune balance. Dysbiosis can increase systemic inflammation that interferes with sleep regulation.
What type of sleep is most affected by inflammation?
Deep (slow-wave) sleep is most vulnerable to inflammatory disruption, even when total sleep time remains unchanged.
Final Thoughts
Chronic inflammation is a strong but often overlooked cause of poor deep sleep. It disrupts immune signals, circadian rhythms, and nervous system balance, which can break up sleep and stop real recovery, even for people who seem to get enough sleep.
Looking at sleep problems in terms of inflammation, gut health, and stress gives a more complete and natural way to improve sleep.
Research from places like the NIH and Stanford Medicine shows that sleep is not just about the brain. It also involves the immune system, metabolism, and gut microbes.