Introduction: Why sleep aids need scientific scrutiny
Insomnia and sleep issues are widespread, affecting memory, mood, health, and productivity. The booming sleep aid market offers supplements, teas, drugs, and devices—all promising better rest.
However, many sleep aids lack strong scientific support.
Some products help with specific sleep problems. Others show only mild, short-term benefits or may pose overlooked risks. To navigate these options, comparing sleep aids through science-backed evidence is essential, allowing people to make informed choices rather than relying on marketing claims or anecdotes.
Building on this approach, this article examines the most common sleep aids—natural, supplemental, pharmaceutical, and behavioral—through the lens of clinical research. You’ll learn what works, what doesn’t, and how to choose the safest and most effective option for your situation.
Understanding insomnia and sleep disorders
Insomnia is not a single condition. Clinically, it includes:
- Difficulty falling asleep
- Difficulty staying asleep
- Waking too early
- Poor sleep quality despite adequate time in bed
Insomnia can be acute (lasting days or weeks) or chronic (lasting three months or more). Common contributing factors include:
- Stress and anxiety
- Irregular schedules or shift work
- Excessive screen exposure
- Medical conditions (pain, reflux, sleep apnea)
- Medications
- Depression or anxiety disorders
Because insomnia has many causes, no single aid works for everyone. This makes research-based comparisons important.
How sleep works: The science behind rest
Sleep occurs in repeating cycles made up of four stages:
- Light sleep (N1 and N2) – The transition from wakefulness into sleep. During these stages, heart rate and body temperature begin to drop, and the brain prepares for deeper sleep.
- Deep sleep (N3) – The most physically restorative stage of sleep. Deep sleep supports tissue repair, muscle growth, immune function, and hormone regulation. Spending adequate time in deep sleep is associated with improved physical recovery and stronger immune resilience.
- REM sleep – The stage most closely linked to dreaming, learning, and emotional processing. REM sleep plays a key role in memory consolidation, creativity, and problem-solving. Consistently getting enough REM sleep supports sharper cognitive performance and emotional balance.
Two biological systems control sleep:
- Circadian rhythm – your internal 24-hour clock is regulated by light exposure.
- Sleep drive – pressure that builds the longer you stay awake.
Hormones like melatonin promote sleepiness, while cortisol promotes alertness. Sleep aids influence these systems in different ways, which explains why some help with falling asleep while others improve sleep quality or duration.
Understanding how sleep works leads to the following key question: What makes a sleep aid effective by scientific standards? Randomized controlled trials set the benchmark, as they compare treatments against a placebo in a controlled environment to yield reliable results. With these criteria, readers can critically judge claims about different sleep aids.
- Effectiveness: Does it improve sleep onset, duration, or quality?
- Consistency: Do results appear across multiple studies?
- Safety: Are side effects or long-term risks present?
- Durability: Do benefits last after stopping use?
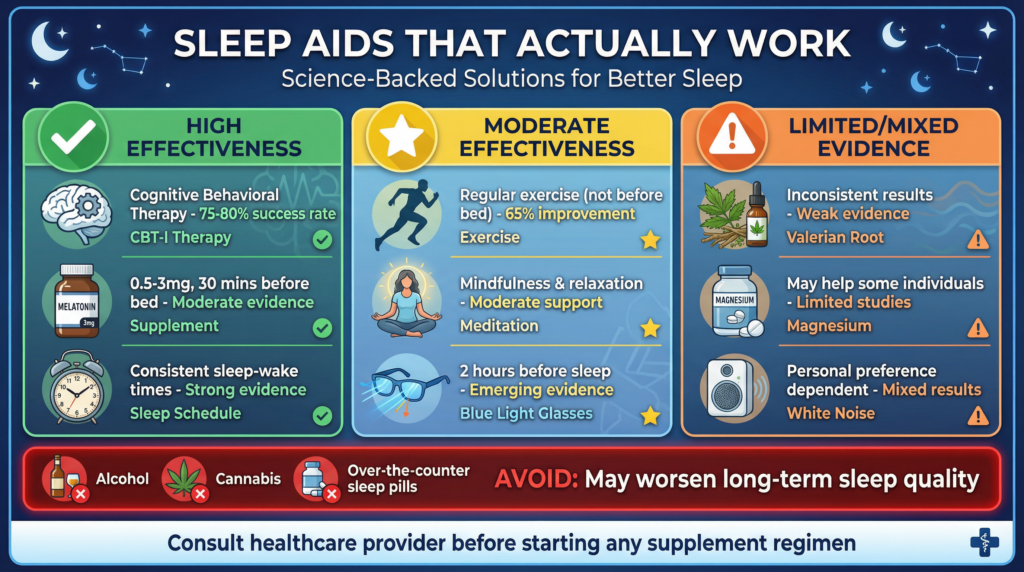
Based on these criteria, sleep aids fall into very different evidence tiers.
Start by understanding which sleep stage you’re missing and why. Small, science-backed changes can make a big difference—begin with one tonight.
👉 Want better sleep without guesswork?
Cognitive Behavioral Therapy for Insomnia (CBT-I): The gold standard
What it is
CBT-I is a structured therapy that addresses the behaviors and thoughts that maintain insomnia. It includes:
- Stimulus control (retraining the bed for sleep only)
- Sleep restriction (consolidating sleep)
- Cognitive restructuring (reducing sleep anxiety)
- Relaxation training
- Sleep hygiene education
What the research shows
Dozens of randomized controlled trials and meta-analyses show CBT-I consistently improves:
- Time to fall asleep
- Night awakenings
- Sleep efficiency
- Daytime functioning
Unlike medications, benefits persist long after treatment ends.
Scientific consensus
Major sleep organizations recommend CBT-I as the first-line treatment for chronic insomnia, even before medication.
Melatonin: Effective for sleep timing, limited for deep insomnia
How melatonin works
Melatonin is a hormone naturally released in the dark. Supplemental melatonin does not sedate the brain; instead, it shifts the timing of sleep.
Scientific evidence
Research consistently shows melatonin:
- Reduces time to fall asleep
- Helps with jet lag and shift-work disorder
- Helps with delayed sleep phase syndrome
However, results are mixed for improving total sleep time or preventing awakenings in chronic insomnia.
Safety considerations
Short-term use is generally safe. Long-term nightly use is still being studied, and dosing above physiological levels may cause next-day grogginess.
Best use: Circadian rhythm problems, not severe insomnia.
Magnesium: Modest benefits with biological plausibility
Why magnesium may help
Magnesium supports nervous system regulation and activates GABA, a calming neurotransmitter. Low magnesium levels are associated with poorer sleep in observational studies.
What studies show
Clinical trials suggest magnesium may:
- Improve subjective sleep quality.
- Reduce nighttime awakenings
- Promote relaxation
Effects tend to be modest and more noticeable in older adults or those with a deficiency.
Forms matter
Magnesium glycinate and magnesium bisglycinate are often better tolerated than magnesium oxide.
CBD (Cannabidiol): Promising but not proven
How CBD affects sleep
CBD interacts with the endocannabinoid system, which influences stress, anxiety, and arousal. It may indirectly help with sleep by reducing anxiety.
Scientific findings
Small randomized trials show mixed results:
- Some improvement in sleep quality and anxiety
- Limited direct sedative effects
- High variability in dosing and response
Large, well-controlled studies are still needed.
Important caution
CBD can interact with medications and varies widely in purity and labeling accuracy.
For those interested in plant-based options, herbal sleep aids like valerian and chamomile are widely used and deserve a closer look.
Valerian root
Research shows small improvements in sleep latency and quality in some studies, but results are inconsistent.
Chamomile
Chamomile contains apigenin, a compound that binds to calming receptors in the brain. Trials suggest mild benefits for people with mild insomnia or anxiety.
Overall evidence
Herbal remedies are generally safe but produce mild and variable effects.
Prescription sleep medications: Effective but risky
Common types
- Benzodiazepines
- Z-drugs (zolpidem, zopiclone, eszopiclone)
Effectiveness
These drugs reliably:
- Reduce sleep onset time.
- Increase total sleep duration.
Risks
- Dependence and tolerance
- Withdrawal insomnia
- Cognitive impairment
- Increased fall risk (especially in older adults)
Medical guidance
Most guidelines recommend short-term use only, combined with behavioral therapy.
Now, it’s useful to directly compare natural and pharmaceutical sleep aids to highlight their unique benefits and dangers.
| Strength of evidence | High for CBT-I | High short-term |
| Long-term safety | High | Lower |
| Risk of dependence | None | Moderate to high |
| Speed of effect | Slower | Fast |
| Durability | Long-lasting | Temporary |
Safety and interaction warnings
- Combining sleep aids can be dangerous.
- Supplements can interact with antidepressants, blood pressure drugs, and sedatives.
- Older adults are more sensitive to sleep medications.
- Pregnancy requires medical supervision.
Always consult a healthcare provider before starting long-term treatment.
FAQs: Comparing sleep aids with science-backed evidence
Q1: What is the safest long-term solution for insomnia?
CBT-I has the strongest long-term safety and effectiveness.
Q2: Is melatonin safe to take every night?
Short-term use is generally safe; long-term nightly use should be medically supervised.
Q3: Can magnesium replace sleeping pills?
Magnesium may help with mild sleep problems, but it is not a substitute for treatment for severe insomnia.
Q4: Does CBD work better than melatonin?
Evidence is weaker and less consistent for CBD compared to melatonin.
Q5: Are herbal sleep aids effective?
They may help mild insomnia, but show small effects in studies.
Q6: Why do doctors avoid long-term sleep medications?
Due to dependence, cognitive risks, and reduced effectiveness over time.
Conclusion: Choosing the right sleep aid wisely
When comparing sleep aids, remember: there is no universal solution. Behavioral therapies provide the most lasting benefits. Supplements target specific sleep issues. Prescription medications work quickly but come with risks.
The most effective approach often combines:
- Behavioral strategies
- Targeted short-term aids
- Medical guidance
The main takeaway: Understanding the science behind sleep aids helps you choose methods that best match your sleep needs, enhancing both short-term sleep quality and long-term health outcomes.
Bookmark this guide and revisit the sleep aid that best matches your symptoms. Better sleep starts with the right approach—not trial and error.
