Introduction
Many believe enough sleep means more time in bed, yet adults often wake exhausted after seven, eight, or nine hours. They may fall asleep quickly, stay in bed, and still feel foggy and low on energy.
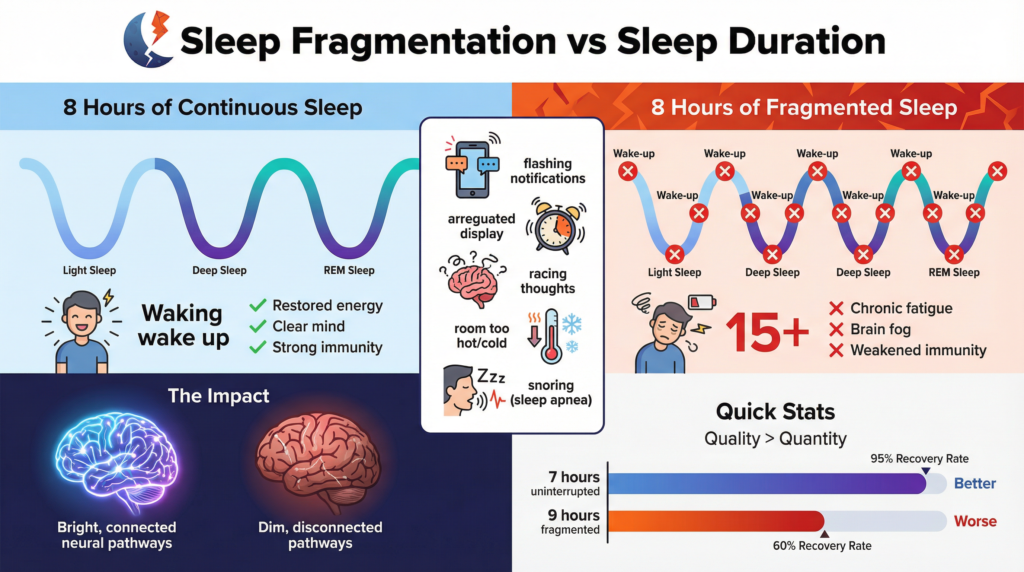
This disconnect is often explained by a critical but overlooked concept: sleep fragmentation.
Sleep quality is not determined solely by duration. What matters just as much, if not more, is how continuous and stable your sleep cycles are throughout the night. Interrupted sleep can prevent the brain and body from entering deep, restorative stages, leaving you tired even after what appears to be a full night’s rest.
Understanding the difference between sleep fragmentation and sleep duration is key to diagnosing persistent fatigue and dealing with sleep problems that don’t improve with standard advice.
Sleep Fragmentation vs Sleep Duration
What is the difference between sleep fragmentation and sleep duration?
Sleep duration refers to the total number of hours you spend asleep.
Sleep fragmentation refers to how often your sleep is interrupted by brief awakenings or movements into lighter sleep stages.
You can sleep eight hours and still be exhausted if your sleep is fragmented. In contrast, shorter but continuous sleep is often more rejuvenating than longer, broken sleep.
What Is Sleep Fragmentation?
Sleep fragmentation occurs when sleep is repeatedly interrupted by:
- Micro-awakenings (often not remembered)
- Shifts from deep sleep to light sleep
- Brief arousals caused by stress, noise, or internal signals
These interruptions may last only seconds, but they are enough to disrupt sleep architecture and prevent sustained deep sleep.
Importantly, most people with broken sleep do not realize they are waking up. Wearable devices and sleep studies often reveal dozens—or even hundreds—of micro-arousals per night.
Watch: Why sleeping 8 hours doesn’t always lead to restorative sleep.
Why Sleep Duration Alone Is a Poor Measure of Sleep Quality
For decades, sleep advice has emphasized “getting enough hours.” While sleep deprivation does impair health, focusing only on duration ignores how sleep actually works.
Sleep Happens in Cycles
Healthy sleep consists of repeated cycles moving through:
- Light sleep (N1, N2)
- Deep sleep (N3)
- REM sleep
Each cycle is about 90 minutes. Fragmentation breaks cycles and forces the brain to restart repeatedly.
When this happens:
- Deep sleep is shortened or eliminated.
- REM sleep becomes unstable
- Sleep becomes lighter as the night progresses.
The result: non-restorative sleep despite adequate hours.
Why You’re Tired After 8 Hours of Sleep
Feeling exhausted after a full night of sleep is one of the most common complaints in sleep medicine. Sleep fragmentation is one of the primary reasons.
Common Signs of Interrupted Sleep
- Morning grogginess or brain fog
- Heavy reliance on caffeine
- Feeling “wired but tired.”
- Poor recovery from exercise
- Irritability or low stress tolerance
These symptoms often persist even when sleep duration appears sufficient.
The Biology of Sleep Fragmentation
Sleep fragmentation is driven by disruptions in the systems that stabilize sleep. These include:
1. Nervous System Hyperarousal
An overactive stress response interrupts sleep. The brain stays partially alert at night, causing more micro-awakenings.
2. Hormonal Disruption
Elevated nighttime cortisol interferes with sleep continuity and deep sleep.
3. Inflammatory Signaling
Cytokines can fragment sleep architecture, even without conscious awakening.
4. Circadian Misalignment
Irregular light exposure, meal timing, or sleep schedules destabilize sleep cycles.
These mechanisms are deeply interconnected and frequently strengthen one another.
Stress and Cortisol as Drivers of Interrupted Sleep
Stress is one of the most powerful contributors to sleep fragmentation. Chronic stress elevates nighttime cortisol, preventing the nervous system from fully shifting into a parasympathetic (rest-and-digest) state.
Elevated cortisol:
- Increases nighttime alertness
- Triggers micro-awakenings
- Shortens deep sleep duration
This relationship is explored in detail in our article on cortisol, stress, and sleep disruption, which explains why stress-driven insomnia often persists even with good sleep hygiene.
Inflammation and Sleep Fragmentation
Chronic inflammation is another major contributor to broken sleep. Inflammatory cytokines interfere with sleep-regulating brain regions and destabilize slow-wave sleep.
Research shows that inflammation:
- Increases nighttime arousals
- Reduces sleep efficiency
- Disrupts REM continuity
This is why individuals with metabolic issues, autoimmune conditions, or chronic stress often experience poor sleep quality despite long sleep duration.
See also: Inflammation and Sleep: How Chronic Inflammation Disrupts Deep Sleep.
The Gut–Brain Axis and Interrupted Sleep
The gut microbiome plays a central role in sleep stability. Through immune signaling, neurotransmitter regulation, and circadian entrainment, gut health influences how consolidated sleep becomes.
Disruptions in gut health can:
- Increase systemic inflammation
- Alter serotonin and GABA signaling.
- Amplify stress responses at night.
These pathways are explored in depth in our pillar guide on gut health and sleep control, which explains why sleep fragmentation often improves when gut balance is restored.
Why Melatonin Doesn’t Fix Interrupted Sleep
Melatonin is commonly used to address sleep problems, but it primarily signals scheduling rather than sleep stability.
Why melatonin often fails:
- It does not suppress stress-driven arousal.
- It does not reduce inflammation.
- It does not restore the continuity of deep sleep.
As discussed in Why Melatonin Stops Working, increasing melatonin without addressing fragmentation may lead to tolerance, vivid dreams, and continued fatigue.
Sleep Fragmentation vs Insomnia: An Important Distinction
Many people with broken sleep do not meet the classic definition of insomnia. They may:
- Fall asleep easily
- Stay in bed all night.
- Believe they are sleeping “fine.”
Yet they wake up exhausted because sleep quality—not sleep onset—is impaired.
This distinction matters because treatments aimed solely at falling asleep may worsen fragmentation.
When to Consider Targeted Sleep Support
You may be dealing with sleep fragmentation if:
- You sleep 7–9 hours yet feel unrefreshed.
- Wearables show low sleep efficiency.
- You wake frequently or feel restless at night.
- Stress or anxiety worsens sleep quality.
- Melatonin hasn’t helped.
In these cases, supporting sleep continuity requires calming the nervous system rather than forcing sleep.
When sleep is fragmented, the issue is often nervous system hyperarousal, not a lack of sleep drive. Supporting relaxation and parasympathetic activity helps stabilize sleep cycles.
We reviewed Yu Sleep through the lens of stress physiology, sleep continuity, and actual recovery data.
Improving Sleep Continuity Naturally
While no single fix resolves broken sleep, several foundational strategies help stabilize sleep cycles:
- Reducing nighttime stress signaling
- Supporting gut health
- Reducing chronic inflammation
- maintaining steady circadian cues
These strategies work together to improve sleep quality even when sleep duration remains unchanged.
Frequently Asked Questions (FAQ)
Can you be sleep deprived even after 8 hours?
Yes. A fragmented sleep cycle can prevent deep and REM sleep, leading to fatigue despite adequate duration.
Is sleep quality more important than sleep duration?
Both matter, but sleep quality—especially continuity and depth—is often the missing factor in chronic fatigue.
What causes micro-awakenings during sleep?
Stress, cortisol, inflammation, gut dysbiosis, and circadian disruption are common causes.
Does melatonin improve sleep fragmentation?
Melatonin helps with timing but does not consistently improve sleep continuity.
How can I tell if my sleep is fragmented?
Symptoms include morning fatigue, frequent night wakings, and low sleep efficiency on wearables.
Can calming the nervous system improve broken sleep?
Yes. Reducing hyperarousal often improves sleep stability and depth.
Conclusion: Why Sleep Quality Matters More Than Sleep Length
When it comes to feeling rested, sleep duration is only part of the equation. You can spend eight hours in bed and still wake up exhausted if your sleep is fragmented by stress, anxiety, frequent awakenings, or an overactive nervous system. In contrast, fewer hours of deep, uninterrupted sleep often feel far more restorative.
This is why many people become frustrated with traditional sleep aids. While they may increase total sleep time, they often fail to improve sleep continuity—and in some cases, they make fragmentation worse by disrupting natural sleep cycles.
Understanding the difference between how long you sleep and how well you sleep is a crucial shift. For chronic insomnia sufferers, especially those who feel tired but wired, the real solution often lies in addressing what’s causing repeated nighttime awakenings rather than simply trying to sleep longer.
Improving sleep quality means focusing on nervous system regulation, reducing nighttime hyperarousal, and choosing approaches that support more profound, more stable sleep—not just sedation.
👉 If you’re sleeping enough hours but still waking up drained, exploring strategies that target sleep fragmentation—not just sleep duration—may be the next logical step toward real rest.
