Did you know that an estimated 1 billion people worldwide have moderate to severe sleep apnea?
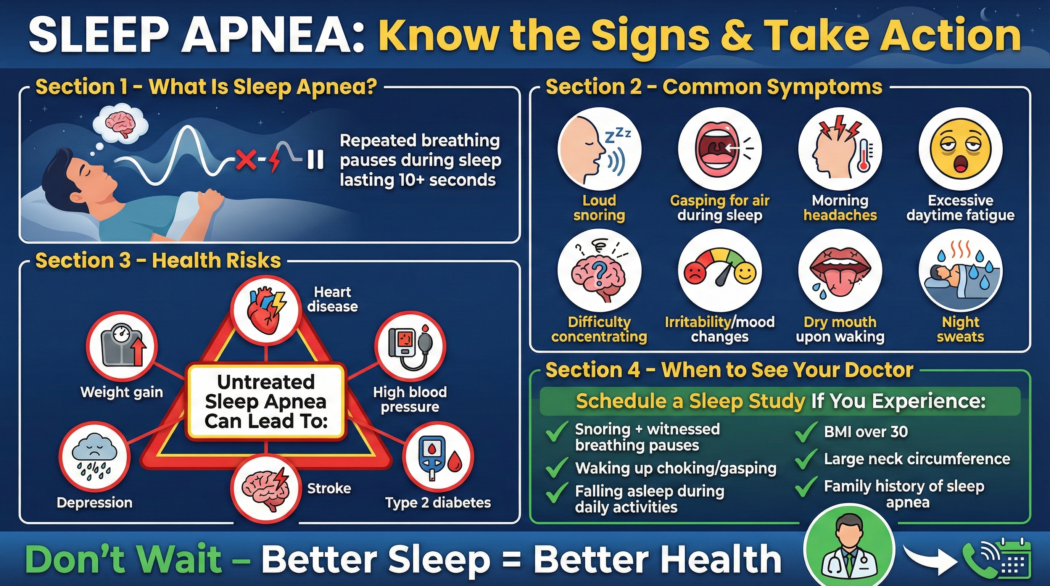
Sleep apnea is a common yet serious sleep disorder that affects millions of people, often without them even realizing it. It’s characterized by repeated interruptions in breathing during sleep. These pauses can last from a few seconds to minutes and may occur many times an hour, disrupting the natural sleep cycle and leading to a cascade of health problems.
Understanding the symptoms, recognizing the risks, and knowing when to seek medical advice are crucial steps toward diagnosis and effective treatment.
What is Sleep Apnea?
At its core, sleep apnea is a condition where your breathing repeatedly stops and starts while you sleep. This isn’t just about snoring loudly; it’s about your airway becoming blocked, either partially or completely, preventing you from getting enough oxygen. When breathing stops, your brain briefly wakes you up to reopen your airway. This often happens so quickly that you don’t remember it, but it significantly disrupts your sleep quality.
There are three main types of sleep apnea:
- Obstructive Sleep Apnea (OSA): The most common type. It occurs when the muscles in the back of your throat relax too much during sleep, causing the soft tissues to collapse and block the airway. Think of it like a hose getting kinked – air can’t flow through.
- Central Sleep Apnea (CSA): This type is less common and occurs when your brain fails to send the proper signals to the muscles that control breathing. Your airway isn’t blocked, but your body simply doesn’t tell itself to breathe.
- Complex Sleep Apnea Syndrome (CompSA): Also known as treatment-emergent central sleep apnea, this condition is a combination of both OSA and CSA. It typically emerges when someone with OSA starts CPAP therapy, and their central apneas then become apparent.
Common Symptoms of Sleep Apnea
Recognizing the signs of sleep apnea is the first step toward getting help. Many symptoms are subtle and can be easily dismissed as just tiredness or stress. However, if several of these symptoms are present, especially together, it’s worth paying attention.
Think Your Sleep Is the Problem — Not Your Bedtime?
Many people with sleep apnea don’t realize their sleep is being disrupted all night long. Before jumping to quick fixes, it helps to understand why your sleep feels broken — even after a full night in bed.
👉 Read next: Why You Wake Up Tired Even After 8 Hours of Sleep (And How to Fix It)
1. Loud and Persistent Snoring
This is perhaps the most well-known symptom. While not everyone who snores has sleep apnea, and not everyone with sleep apnea snores loudly, loud, disruptive snoring is a significant red flag. The snoring is often characterized by pauses in breathing followed by a sudden gasp or snort as the airway reopens. This can be so loud that it disturbs a bed partner.
2. Episodes of Stopped Breathing During Sleep
This is the defining characteristic of sleep apnea, though it’s often witnessed by a sleep partner rather than the person experiencing it. These episodes, called apneas, are moments when breathing ceases for 10 seconds or longer. When they occur, the brain signals the body to wake up just enough to resume breathing, often with a choking or gasping sound.
3. Excessive Daytime Sleepiness (EDS)
Even if you believe you’re getting enough hours of sleep, uncontrollable sleepiness during the day is a hallmark symptom. You might find yourself dozing off at work, while driving, or even during conversations. This isn’t just feeling a bit tired; it’s an overwhelming urge to sleep that can interfere with daily activities and safety.
4. Morning Headaches
Waking up with a headache, especially a dull, throbbing one, can be a sign of sleep apnea. This is often attributed to the reduced oxygen levels in the blood and the buildup of carbon dioxide during the night. As your body struggles to breathe, these imbalances can manifest as headaches.
5. Difficulty Concentrating and Memory Problems
Sleep is crucial for cognitive function, including concentration, memory, and decision-making. The fragmented sleep caused by sleep apnea can lead to problems with focus, attention, and recall. You might find yourself more forgetful, easily distracted, or struggling to perform tasks that require mental effort.
6. Irritability and Mood Swings
Lack of quality sleep can significantly impact your emotional well-being. People with sleep apnea often experience increased irritability, moodiness, and even symptoms of depression or anxiety. The constant struggle for breath and the resulting sleep deprivation can take a toll on mental health.
7. Waking Up with a Dry Mouth or Sore Throat
Breathing through your mouth during sleep, often a consequence of airway obstruction, can lead to a dry mouth and a sore throat upon waking. This is because the mouth and throat tissues become dehydrated.
8. Frequent Urination at Night (Nocturia)
While not as commonly known, some individuals with sleep apnea experience the urge to urinate multiple times during the night. This can be related to changes in chest pressure and hormone levels that occur when breathing is interrupted.
9. Restless Sleep
Even if you don’t remember waking up, frequent micro-arousals from sleep apnea can lead to overall restless sleep. You might wake up feeling unrefreshed, as if you haven’t slept at all.
The Serious Health Risks of Untreated Sleep Apnea
Sleep apnea is far more than just an inconvenience; it’s a serious medical condition that, if left untreated, can have profound and potentially life-threatening consequences. Repeated drops in oxygen levels and constant stress on the body disrupt vital bodily functions and increase the risk of numerous health problems.
1. Cardiovascular Problems
One of the most significant risks associated with sleep apnea is its impact on heart health. The repeated oxygen deprivation and the surges in blood pressure during apneas put immense strain on the cardiovascular system. This can lead to:
- High Blood Pressure (Hypertension): Sleep apnea is a common cause of secondary hypertension. The body releases stress hormones in response to the breathing interruptions, which constrict blood vessels and raise blood pressure. According to the American Heart Association, people with OSA are significantly more likely to develop hypertension.
- Heart Disease: Untreated sleep apnea increases the risk of coronary artery disease, heart attacks, and heart failure. The chronic stress on the heart can lead to structural changes and reduced pumping efficiency.
- Stroke: The link between sleep apnea and stroke is well-established. Reduced oxygen supply to the brain and increased blood pressure can contribute to the formation of blood clots and damage to blood vessels in the brain.
- Arrhythmias (Irregular Heartbeats): Conditions like atrial fibrillation are more common in individuals with sleep apnea.
2. Type 2 Diabetes
There’s a strong connection between sleep apnea and insulin resistance, a precursor to type 2 diabetes. The stress hormones released during apneas can interfere with the body’s ability to use insulin effectively. Furthermore, disrupted sleep can affect glucose metabolism. Research published in the Journal of Clinical Endocrinology & Metabolism has shown a significant association between sleep apnea and impaired glucose tolerance.
3. Metabolic Syndrome
Metabolic syndrome is a cluster of conditions that increase the risk of heart disease, stroke, and diabetes. These conditions include high blood pressure, high blood sugar, unhealthy cholesterol levels, and excess abdominal fat. Sleep apnea is considered a contributing factor to the development of metabolic syndrome.
4. Liver Problems
Studies have indicated a link between sleep apnea and nonalcoholic fatty liver disease (NAFLD). The intermittent hypoxia (low oxygen) and sleep fragmentation associated with sleep apnea can contribute to liver inflammation and damage.
5. Increased Risk of Accidents
Excessive daytime sleepiness is not just a symptom; it’s a major safety hazard. Drowsiness significantly impairs reaction time, judgment, and awareness, increasing the risk of:
- Motor Vehicle Accidents: Driving while drowsy can be as dangerous as driving under the influence of alcohol. The National Highway Traffic Safety Administration (NHTSA) estimates that drowsy driving causes thousands of crashes each year.
- Workplace Accidents: Impaired alertness can lead to mistakes and accidents, especially in jobs that require concentration or the operation of machinery.
6. Complications with Medications and Surgery
Sleep apnea can complicate medical procedures. Anesthesia and sedatives used during surgery can worsen airway obstruction and breathing problems, increasing the risk of complications during and after surgery. It’s crucial for your medical team to be aware of any sleep apnea diagnosis.
7. Depression and Anxiety
As mentioned earlier, chronic sleep deprivation and the stress of dealing with the disorder can exacerbate or contribute to mental health issues like depression and anxiety. The feeling of not being able to get restful sleep can be incredibly demoralizing.
8. Poor Quality of Life
Ultimately, untreated sleep apnea significantly diminishes a person’s overall quality of life. The constant fatigue, cognitive impairment, mood disturbances, and health complications can make it difficult to enjoy work, relationships, and daily activities.
Before You Book a Sleep Study, Try This First
If your sleep apnea symptoms are mild to moderate, small changes in sleep environment and nighttime breathing support can make a noticeable difference.
Many readers start with a non-invasive sleep solution designed to reduce nighttime disruptions and promote deeper, more stable sleep — without machines or prescriptions.
👉 Explore the natural sleep support many people try before CPAP therapy
When to Ask Your Doctor About a Sleep Study
If you’re experiencing any of the symptoms listed above, especially if they are persistent and impacting your daily life, it’s time to consider talking to your doctor about a sleep study. A sleep study, also known as a polysomnography (PSG), is the definitive way to diagnose sleep apnea.
Signs That Warrant a Doctor’s Visit:
- You have a bed partner who reports that you snore loudly, gasp for air, or stop breathing during sleep. This direct observation is a powerful indicator.
- You experience excessive daytime sleepiness that interferes with your work, social life, or safety (e.g., falling asleep while driving).
- You wake up with frequent headaches, especially in the morning.
- You have been diagnosed with or suspect you have other health conditions strongly linked to sleep apnea, such as high blood pressure, heart disease, type 2 diabetes, or atrial fibrillation.
- You have a higher risk profile for sleep apnea. Factors include being overweight or obese, having a large neck circumference, a history of stroke, or certain facial anatomical features (like a recessed chin or large tongue).
- You’ve tried to improve your sleep hygiene (e.g., a consistent bedtime and a dark room), but you still feel unrefreshed and excessively sleepy during the day.
What to Expect During a Sleep Study:
A sleep study is a non-invasive test that monitors your body’s functions during sleep. It’s typically conducted overnight in a sleep center, though home sleep apnea tests (HSATs) are available for some individuals.
During a polysomnography at a sleep center, you can expect:
- Electrodes: Small sensors will be attached to your scalp, face, and chin to record brain waves, eye movements, and muscle activity. These help determine sleep stages.
- Chest and Abdomen Bands: These measure your breathing effort.
- Nasal Cannula: A small tube under your nose monitors airflow.
- Pulse Oximeter: A clip, usually on your finger or earlobe, measures your blood oxygen levels.
- Microphone: Records snoring.
- Video Monitoring: Your sleep is often recorded on video to note body movements.
The data collected helps doctors determine if you have sleep apnea, its severity, and its type.
Seeking Professional Help
Don’t dismiss persistent sleepiness or loud snoring as normal. These can be signs of a serious condition that, with proper diagnosis and treatment, can be managed effectively. If you suspect you or a loved one has sleep apnea, the best course of action is to consult your primary care physician. They can assess your symptoms and medical history and refer you to a sleep specialist if a sleep study is recommended.
What is Sleep Hygiene and How Can It Help?
While sleep hygiene is not a cure for sleep apnea, practicing good sleep habits can support overall sleep quality and complement medical treatments. Good sleep hygiene includes:
- Maintaining a consistent sleep schedule: Go to bed and wake up around the same time each day, even on weekends.
- Creating a relaxing bedtime routine: This could include reading, taking a warm bath, or listening to calming music.
- Ensuring your bedroom is dark, quiet, and cool: Optimize your sleep environment.
- Avoiding caffeine and alcohol close to bedtime: These substances can disrupt sleep.
- Limiting screen time before bed: Blue light from electronic devices can interfere with melatonin production.
For individuals struggling with sleep issues, understanding what actually fixes chronic insomnia can provide valuable insights, even though sleep apnea requires a different diagnostic and treatment approach. What actually fixes chronic insomnia is a great resource for understanding broader sleep health principles.
Conclusion
Sleep apnea is a pervasive and dangerous sleep disorder that demands attention. Its symptoms, from disruptive snoring and daytime fatigue to more serious health implications like heart disease and diabetes, underscore the importance of early detection. If you recognize these signs in yourself or a loved one, don’t hesitate to discuss the possibility of a sleep study with your doctor. A diagnosis is the first step toward reclaiming restful sleep and protecting your long-term health. Investing in your sleep is investing in your life.
Frequently Asked Questions (FAQs)
Q1: Can sleep apnea be cured?
A1: While sleep apnea cannot be “cured” in the sense of being permanently eradicated, it is highly treatable. The most common treatment, Continuous Positive Airway Pressure (CPAP) therapy, is very effective at managing the condition and restoring normal breathing during sleep. Other treatments, such as oral appliances, lifestyle changes, and, in some cases, surgery, can also be effective depending on the type and severity of sleep apnea.
Q2: Is sleep apnea only a problem for overweight people?
A2: While being overweight or obese is a significant risk factor for Obstructive Sleep Apnea (OSA), it is not the only cause. People of all body weights can develop OSA. Other factors, such as jaw structure, neck circumference, age, gender, and genetics, also play a role. Central Sleep Apnea (CSA) is often related to underlying medical conditions and is not typically linked to weight.
Q3: How can I tell if my snoring is serious enough to warrant a sleep study?
A3: Not all snoring indicates sleep apnea. However, if your snoring is very loud, often described as disruptive, and is accompanied by pauses in breathing, gasping or choking sounds during sleep, or excessive daytime sleepiness, it’s a strong sign that you should consult a doctor about a sleep study. Your bed partner’s observations are often key.
Q4: What are the main differences between Obstructive Sleep Apnea (OSA) and Central Sleep Apnea (CSA)?
A4: The primary difference lies in the cause of the breathing interruption. In OSA, the airway physically collapses or becomes blocked. In CSA, the brain fails to send the correct signals to the muscles that control breathing. OSA is far more common and often linked to physical factors like excess weight, while CSA is usually associated with other medical conditions like heart failure or stroke.
Q5: Can children have sleep apnea?
A5: Yes, children can and do develop sleep apnea. In children, OSA is often caused by enlarged tonsils or adenoids, but other factors can also contribute. Symptoms in children can include loud snoring, mouth breathing, difficulty sleeping, daytime fatigue, behavioral issues, and poor growth. If you suspect your child has sleep apnea, it’s important to consult a pediatrician.
Q6: Are home sleep apnea tests (HSATs) as accurate as in-lab polysomnography?
A6: Home sleep apnea tests (HSATs) are generally accurate for diagnosing moderate to severe OSA in individuals with a high probability of having the disorder. However, they typically monitor fewer parameters than in-lab polysomnography (PSG). PSG is considered the gold standard for diagnosing complex sleep apnea, central sleep apnea, and other sleep disorders. Your doctor will determine if an HSAT or an in-lab PSG is most appropriate for you.
Better Sleep Starts With the Right First Step
Sleep apnea symptoms are your body’s way of asking for attention — not panic. Whether you need a sleep study or simply better nighttime support, the goal is the same: consistent, restorative sleep.
If you’re looking for a gentle, non-invasive way to support deeper sleep while you figure out your next step, this is where many readers begin.
👉 Discover the sleep support that helps calm nights and clearer mornings
External Resources:
- National Heart, Lung, and Blood Institute (NHLBI): Offers comprehensive information on sleep apnea, its causes, symptoms, and treatments. https://www.nhlbi.nih.gov/health/sleep-apnea
- American Academy of Sleep Medicine (AASM): Provides patient resources, fact sheets, and information on sleep disorders, including sleep apnea. https://aasm.org/
- Centers for Disease Control and Prevention (CDC): Discusses the health effects of sleep apnea and provides statistics on its prevalence. https://www.cdc.gov/sleep/about_sleep/sleep_apnea.html
