If you’ve been struggling with insomnia for months—or even years—you’ve likely asked yourself the same question countless times:
Why can’t I sleep when I’m exhausted?
You’ve tried earlier bedtimes. Better sleep hygiene. Supplements. Sleep aids. Maybe even prescription medication. And yet, sleep still feels fragile, shallow, or unpredictable.
That’s because chronic insomnia is rarely caused by a lack of sleep opportunity.
It’s caused by systems in the body that no longer know how to shut down at night.
This page explains the root causes of chronic insomnia, so you can stop guessing and finally learn what helps. Plus, it provides practical steps and actionable strategies to address these causes, ensuring that the information is not only theoretical but also applicable to your daily life.
Why Insomnia Becomes Chronic (And Doesn’t Just “Go Away”)
Acute insomnia is common. Chronic insomnia is different.
Acute insomnia is usually triggered by:
- Temporary stress
- Illness
- Schedule disruption
- Travel
Chronic insomnia develops when the body learns to stay awake.
After weeks or months of poor sleep:
- The brain associates night with threat
- The nervous system stays alert after dark.
- Increased sleep effort worsens arousal.
At this point, insomnia is no longer about sleep habits.
At this stage, insomnia is mainly caused by ongoing alertness of the mind and body, known as conditioned hyperarousal. This occurs when the body’s alert systems become overly responsive at night, often due to repeated stressors or an enduring state of vigilance, making it difficult for the mind and body to relax and achieve restful sleep.
Nervous System Hyperarousal: The Core Driver of Chronic Insomnia
At the center of chronic insomnia is a nervous system that won’t fully shut down.
This often looks like:
- Racing thoughts at bedtime
- A “wired but tired” feeling
- Light, easily disrupted sleep.
- Frequent nighttime awakenings
- Early morning anxiety
Even when you’re exhausted, your body doesn’t feel safe enough to sleep deeply.
This is why insomnia is so commonly linked to:
- Chronic stress
- Anxiety
- Perfectionism
- Overthinking
- Long-term pressure
👉Anxiety-Driven Insomnia: Why Your Brain Won’t Shut Off at Night
Sleep Fragmentation vs Sleep Duration: Why Hours Don’t Equal Rest
One of the biggest misconceptions about sleep is that more hours automatically mean better sleep.
In reality, sleep quality matters far more than sleep length.
Many people with insomnia:
- Sleep 7–8 hours
- Wake multiple times
- Never reach deep, restorative sleep.
- Feel exhausted despite “enough” sleep.
This persistent disruption of sleep quality is called sleep fragmentation, meaning your sleep is broken up by frequent awakenings.
Sleep aids often increase sleep hours, but may worsen fragmentation. That’s why many say, “I slept longer, but I feel worse.”
Also read: Sleep Fragmentation vs Sleep Duration
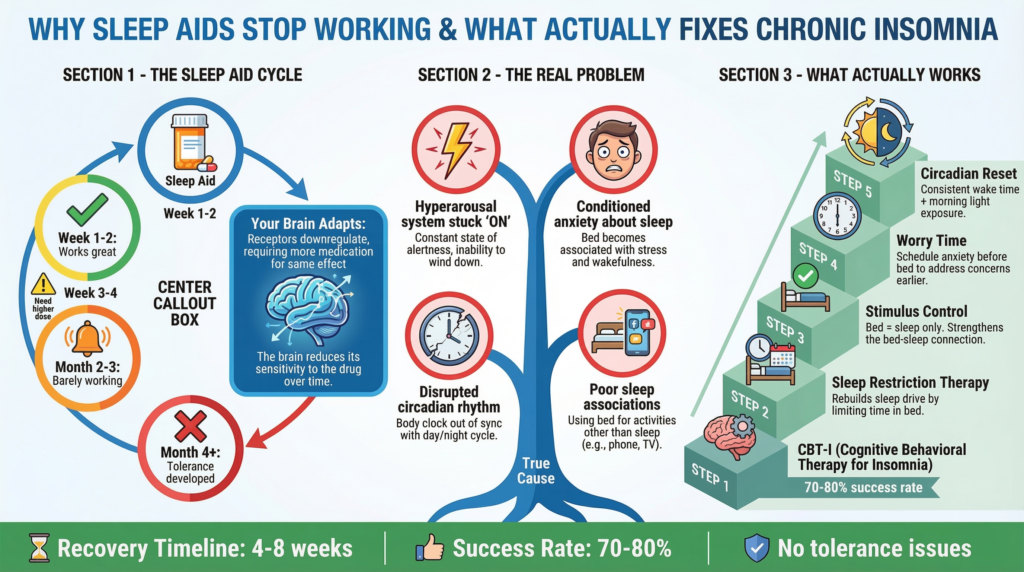
Why Sleep Aids Stop Working Over Time
Sleep aids are usually the first line of defense—and the first major disappointment.
They often work briefly because they increase sedation.
But sedation is not the same as restorative sleep.
Over time, sleep aids fail due to:
- Tolerance (the brain adapts quickly)
- Rebound insomnia (hyperarousal when the aid wears off)
- Suppressed deep sleep
- Increased anxiety about sleep
This is especially true with:
- Antihistamines
- High-dose melatonin
- Prescription sedatives
👉 Why Sleep Aids Stop Working (And What Actually Fixes Chronic Insomnia
Circadian Rhythm Disruption (Shift Work, Jet Lag, Late Nights)
Not all insomnia starts with anxiety.
Circadian disruption is common in:
- Shift workers
- Frequent travelers
- Night owls are forced into early schedules.
- People are using melatonin incorrectly.
When sleep timing is misaligned:
- The body releases alertness hormones at night.
- Melatonin timing becomes erratic.
- Sleep pressure builds at the wrong hours.
High-dose melatonin often makes this worse rather than better.
👉 Melatonin vs Diphenhydramine vs Doxylamine: Which OTC Sleep Aid Is Strongest?
Gut Health, Inflammation, and the Sleep Connection
Sleep isn’t controlled only by the brain—it’s influenced by the gut.
The gut–brain axis affects:
- Inflammation
- Neurotransmitter production
- Stress hormone signaling
When gut health is compromised:
- Cortisol remains elevated at night.
- Anxiety increases
- Sleep becomes lighter and more fragmented.
This explains why many people experience insomnia alongside:
- Digestive issues
- Chronic stress
- Inflammation
👉 Gut Health and Sleep: The Microbiome–Insomnia Connection
Why “Strongest Sleep Aid” Thinking Backfires
When sleep doesn’t improve, many people search for stronger solutions.
But stronger sedation often means:
- More next-day fog
- Worse sleep architecture
- Greater dependence
- Higher anxiety over time
This is especially risky for adults over 40.
👉Strongest Sleep Aid Over the Counter: What Really Works?
What Actually Helps Chronic Insomnia Long-Term
Across research and real-life experience, chronic insomnia improves when people stop forcing sleep and start reducing nighttime hyperarousal. What helps:
- Calming the nervous system before bed, improving sleep continuity
- Reducing anxiety around sleep, supporting natural sleep transitions
- Addressing the underlying causes rather than just the symptoms. Change typically takes time, but improvement comes
when the right factors that influence sleep are addressed.
Where Non-Pill Approaches Fit In
Because chronic insomnia is often driven by hyperarousal, many people explore non-pill approaches that focus on calm rather than sedation.
These approaches aim to:
- Reduce nervous system alertness. Improve sleep by avoiding forced sedation.
- Avoid tolerance and dependency.
- Support long-term improvement
They’re not instant fixes, but often succeed where sleep aids fail.
👉 If pills and supplements haven’t solved your insomnia, a non-pill created to aid in supporting nighttime calm may be worth exploring.
Choosing the Right Next Step (Without Guesswork)
There is no single solution for everyone, but there is a logical progression. To facilitate this, consider a brief self-assessment to identify your primary driver of insomnia. Ask yourself questions like: What situations or thoughts are keeping me awake? Is anxiety playing a role? Am I waking up frequently, or is it an issue with bedtime? Recognizing the main contributors to your sleep issues can help guide your approach more effectively.
- Identify the dominant root cause (anxiety, fragmentation, circadian issues, inflammation)
- Choose approaches aligned with that cause.
- Avoid escalating sedation
When people follow this sequence, sleep often improves naturally.
Final Thoughts: Chronic Insomnia Is a System Problem
Chronic insomnia is not a personal failure.
It’s not a willpower issue.
And it’s rarely fixed by stronger sleep aids.
It’s a systems problem—one involving the nervous system, the brain, the body, and the environment.
Once you understand why sleep stopped working, the path becomes clearer—and far less overwhelming.
Tired of Trying Everything for Insomnia? Try What Works. Most sleep aids just mask symptoms — Yusleep helps rebalance your sleep cycle from the inside out.🌿 Clinically backed. Non-habit forming. Real results.
